What is a knee fracture?
What is a knee fracture?
A knee fracture refers to a break in any of the bones that make up the knee joint, which includes the femur (thigh bone), tibia (shin bone), and fibula (smaller bone in the lower leg).
Knee fractures are serious injuries and often require surgery to heal. Over the long term, they may cause arthritis in the knee.
OrthoConnecticut’s team of board-certified, fellowship-trained knee specialists have extensive experience diagnosing and repairing knee fractures. We offer state-of-the art treatment and the convenience of both surgery and follow-up care in a local setting.
What causes knee fractures?
Knee fractures can be caused by various factors, including:
- Traumatic injury: One of the most common causes of knee fractures is a traumatic injury, such as a fall, sports-related accident, or motor vehicle collision. The impact can exert excessive force on the knee joint, leading to fractures in the bones.
- Direct blow: A direct blow to the knee, such as being struck by a heavy object, can cause fractures in the bones of the knee joint. This type of injury often occurs in contact sports or accidents.
- Osteoporosis: Weakening of the bones due to osteoporosis can make them more prone to fractures, including in the knee joint. Osteoporosis is a condition characterized by low bone density and increased risk of fractures.
- Repetitive stress: Overuse or repetitive stress on the knee joint, especially in activities that involve repetitive bending or twisting of the knee, can lead to stress fractures. These fractures are small cracks in the bone that can gradually develop over time.
- Aging: As we age, the bones can become weaker and more brittle, making them more susceptible to fractures. Older adults may experience knee fractures due to a fall or even a minor injury that wouldn’t have caused a fracture in younger individuals.
- Medical conditions: Certain medical conditions, such as bone tumors or infections, can weaken the bones and increase the risk of fractures in the knee joint.
What are the symptoms of a knee fracture?
The symptoms of a knee fracture can vary depending on the location and severity of the fracture. Here are some common symptoms that may be experienced:
- Pain: Intense pain in the knee is a primary symptom of a fracture. The pain may be severe and worsen with movement or weight-bearing activities.
- Swelling: Swelling around the knee joint is a typical response to injury, including fractures. The swelling may be localized or spread throughout the knee area.
- Bruising: The presence of bruising, also known as discoloration or contusion, around the knee is a common symptom. It occurs due to the accumulation of blood beneath the skin as a result of the fracture.
- Deformity: In some cases, a knee fracture can cause visible deformity or misalignment of the knee joint. The knee may appear bent at an abnormal angle or have an obvious change in shape.
- Difficulty bearing weight: A knee fracture can make it challenging or impossible to bear weight on the affected leg. Walking or putting pressure on the knee joint may cause severe pain and instability.
- Limited range of motion: Knee fractures can restrict the normal range of motion of the knee joint. You may have difficulty bending or straightening the knee fully.
- Tenderness: The knee may feel tender to the touch, and pressure applied to the area may elicit pain.
Types of Knee Fractures
There are several types of knee fractures, each involving different bones and areas within the knee joint. The specific type of fracture can impact the treatment approach and the potential for complications. Here are some common types of knee fractures:
Patellar fractures
Patellar fractures occur in the kneecap (patella), which is the bone in the front of the knee joint. Patellar fractures can be either partial or complete and may result from direct trauma or a sudden contraction of the quadriceps muscle. These fractures can be displaced (where the bone fragments are not in their normal position) or non-displaced.
Femur fractures
Femur fractures are fractures of the thigh bone, which is the bone that connects the hip to the knee. Femur fractures may happen in the upper third, middle third, or lower third of the bone.
Avulsion fractures
Avulsion fractures occur when a small fragment of bone is pulled away from its attachment site by a strong ligament or tendon. In the knee, avulsion fractures can involve the patellar tendon, quadriceps tendon, or collateral ligaments. These fractures are often caused by sudden, forceful muscle contractions or twisting motions.
Tibia fractures
Tibia fractures are fractures of the shin bone, which is the bone that connects the knee to the ankle. Tibia fractures may occur in the upper third, middle third, or lower third of the bone.
Fibula fractures are fractures of the smaller bone in the lower leg, which is located on the lateral (outside) aspect of the knee. Fibula fractures may occur in the upper third, middle third, or lower third of the bone.
Distal femoral fractures
Distal femoral fractures are fractures that occur at the distal end of the femur, which is the end closest to the knee. These fractures frequently involve the articular surface of the knee, which can lead to significant joint instability.
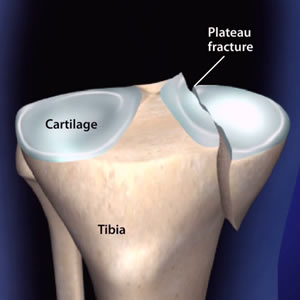
Proximal tibial fractures
Proximal tibial fractures are fractures that occur at the proximal end of the tibia, which is the end closest to the knee. These fractures can also involve the articular surface of the knee, which can lead to significant joint instability.
All these types of fractures can be caused by a variety of reasons, such as high-impact injuries, falls, or overuse. They can lead to pain, swelling, stiffness, and difficulty moving the knee. Depending on the severity of the fracture, treatment may include rest, physical therapy, bracing, or surgery.
How are knee fractures diagnosed?
To diagnose a knee fracture, a healthcare professional will typically perform a comprehensive evaluation that includes the following steps:
Medical history and physical examination
The doctor will ask about your symptoms, how the injury occurred, and any relevant medical history. They will also conduct a physical examination of your knee, assessing for pain, swelling, deformity, range of motion, and stability.
Imaging tests
Various imaging tests are commonly used to confirm the presence of a knee fracture and evaluate its extent. These may include:
- X-rays: X-rays provide detailed images of the bones and can often reveal fractures, their location, and any displacement or misalignment of the bones.
- MRI (Magnetic Resonance Imaging): MRI uses magnetic fields and radio waves to generate detailed images of the knee joint, including the bones, soft tissues, and ligaments. It can help assess the extent of the fracture, evaluate associated injuries, and identify any damage to surrounding structures.
- CT (Computed Tomography) scan: In some cases, a CT scan may be ordered to obtain more detailed images of the knee joint. CT scans can provide cross-sectional images, allowing for a more comprehensive evaluation of complex fractures.
- Additional tests: Depending on the specific circumstances and suspected injuries, additional tests such as ultrasound or bone scans may be ordered to further assess the knee joint and surrounding tissues.
Once the diagnosis of a knee fracture is confirmed, the healthcare professional will determine the appropriate treatment plan, which may involve conservative management (e.g., casting, bracing, or immobilization) or surgical intervention (e.g., internal fixation, external fixation, or joint replacement). The treatment approach will depend on factors such as the type of fracture, its location, stability, and associated injuries.
How long does it take to recover from a knee fracture?
The recovery time for a knee fracture can vary depending on several factors, including the type and severity of the fracture, the individual’s overall health, age, and adherence to the treatment plan. In general, the recovery period for a knee fracture can range from a few weeks to several months. Here is a rough timeline of the recovery stages:
Immediate post-injury phase
In the first few days following the fracture, the focus is on managing pain and swelling. Immobilization of the knee joint using a cast, brace, or splint may be necessary. Weight-bearing and movement of the affected leg may be restricted.
Healing phase
The bones begin to heal during this phase, which usually takes about 6 to 8 weeks. The exact duration can vary depending on the type and location of the fracture. During this time, the individual may gradually start physical therapy exercises to maintain joint mobility, prevent muscle stiffness, and promote blood circulation.
Rehabilitation phase
After the initial healing phase, rehabilitation plays a crucial role in restoring strength, flexibility, and function to the knee joint. Physical therapy exercises are tailored to the individual’s specific needs, and the duration of this phase can range from several weeks to a few months. The goal is to regain full range of motion, improve muscle strength and stability, and gradually return to normal activities and functional movements.
It’s important to note that the recovery timeline is approximate, and individual variations exist. Some factors that can affect the recovery time include the presence of associated injuries, complications, the need for surgical intervention, and the overall health and commitment to rehabilitation.
What complications can occur with knee fracture?
Knee fractures can sometimes be associated with complications, particularly if not properly treated or managed. Some potential complications that can arise from a knee fracture include:
Delayed healing or nonunion
In some cases, the fractured bones may not heal properly or may take longer than expected to heal. This is known as delayed healing or nonunion. Factors such as poor blood supply to the area, inadequate immobilization, or certain medical conditions can contribute to this complication.
Malunion
Malunion occurs when the fractured bones heal in an improper position or alignment. This can result in deformity, altered joint mechanics, and potential long-term functional limitations.
Infection
Any open fractures or surgical interventions to treat the fracture can increase the risk of infection. Infections can lead to prolonged healing time, increased pain, swelling, and may require additional treatment such as antibiotics or surgical intervention to address the infection.
Knee stiffness
Immobilization, lack of movement, or prolonged periods of non-weight bearing can lead to knee stiffness or loss of range of motion. Physical therapy and rehabilitation are crucial to restore mobility and prevent long-term stiffness.
Cartilage damage
Fractures that involve the articular surface of the knee joint can result in cartilage damage. This can lead to ongoing joint pain, instability, and potentially increase the risk of developing degenerative conditions like osteoarthritis in the future.
Nerve or blood vessel injury
Severe knee fractures may injure the surrounding nerves or blood vessels. This can result in numbness, tingling, weakness, or vascular complications that require immediate medical attention.
Compartment syndrome
In some cases, severe fractures combined with significant soft tissue swelling can lead to compartment syndrome. This condition occurs when pressure builds up within a muscle compartment, compromising blood flow and potentially causing tissue damage. Compartment syndrome is a medical emergency that requires prompt intervention.
Can knee fractures lead to long term problems?
Knee fractures can lead to long-term problems or complications that can impact the function and overall health of the knee joint. Some potential long-term problems that can arise from knee fractures include:
Post-Traumatic Osteoarthritis
Knee fractures, especially those involving the articular surface or cartilage, can increase the risk of developing post-traumatic osteoarthritis. The damage to the cartilage and joint structures can lead to joint degeneration over time, causing chronic pain, stiffness, and reduced mobility.
Persistent pain
Even after the fracture has healed, some individuals may experience persistent pain in the knee joint. This can be due to factors such as nerve damage, malalignment, residual cartilage damage, or the development of arthritis.
Limited range of motion
Stiffness and limited range of motion can be long-term consequences of knee fractures, particularly if adequate rehabilitation and physical therapy are not undertaken. Adhesions, muscle imbalances, and joint contractures can restrict the ability to fully bend or straighten the knee.
Instability and weakness
Fractures that involve ligament or tendon damage can result in long-term instability and weakness in the knee joint. This can affect overall joint function, stability during physical activities, and may increase the risk of recurrent injuries.
Functional limitations
Depending on the severity and location of the fracture, long-term functional limitations may arise. These can include difficulty with activities such as walking, running, climbing stairs, or participating in sports or physical activities that require full knee function.
Psychological impact
Long-term problems resulting from a knee fracture can have psychological effects, such as decreased confidence, fear of reinjury, or a negative impact on overall quality of life.
Treatment of Knee Fractures
The treatment for knee fractures depends on the severity and type of fracture. Here are some common treatment options:
Immobilization
For minor fractures, the knee may be immobilized with a brace, cast, or splint to allow the bones to heal properly. The period of immobilization can vary based on the specific fracture and the advice of the treating physician.
Non-Surgical Management
Some knee fractures can be managed without surgery, especially if the bones are not significantly displaced or if the fracture involves only a small piece of bone. In such cases, the treatment may involve rest, pain management with medications, physical therapy, and gradual weight-bearing as the fracture heals.
Surgical Intervention
In more severe cases, surgical intervention may be necessary to realign the fractured bones and stabilize the knee joint. The surgical options can include the following:
- Internal fixation: This involves the use of screws, plates, or rods to hold the fractured bones in place while they heal.
- External fixation: In certain complex fractures, external fixation devices may be used to stabilize the knee joint. These devices are placed outside the body and connected to the bones with pins or wires.
- Knee arthroscopy: This minimally invasive procedure may be used to treat certain types of knee fractures, particularly those involving the surface of the joint. The surgeon uses small instruments and a camera inserted through tiny incisions to repair the fracture.
Rehabilitation
Regardless of the treatment method used, rehabilitation plays a crucial role in recovering from a knee fracture. Physical therapy is typically recommended to help restore knee mobility, strengthen the surrounding muscles, and improve overall function. The specific rehabilitation program will depend on the nature of the fracture and the individual patient’s needs.

 What is a knee fracture?
What is a knee fracture?